Cancer Treatment
Histotripsy can be used for non-invasive tumor ablation for a broad range of cancer applications, including tumors in the pancreas, kidney, breast, prostate, uterus, thyroid, and brain. Currently, we are focusing on liver tumors and brain tumors. We are current focusing on developing histotripsy for treatment of liver tumors and brain tumors.
Liver tumor treatment
Primary liver cancer is a leading cause of cancer morbidity and mortality worldwide, accounting for >600,000 deaths each year. Approximately 85% of patients with liver tumors are not eligible for surgical resection, and in many of these patients, ablation is an important option. The most widely applied thermal ablation techniques, including radiofrequency and microwave ablation, have inherent drawbacks that can limit effectiveness and the applicable patient population. High intensity focused ultrasound (HIFU) is a non-invasive ultrasound thermal ablation method with drawbacks related to the heat sink effect, anatomic challenges such as ablating through ribs and respiratory motion, and long procedure times, thus resulting in rare clinical use.
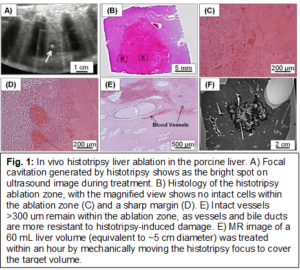
We have obtained substantial in vivo data in porcine normal liver1-4 to show the following (Fig. 1): (1) consistent cellular disruption in the target through intact ribs and other tissue without damage along the energy delivery path; (2) sharp margins <1 mm without significant inflammation; (3) capability to ablate tumors of any shape, size, and nodule number; (4) complete ablation of a 60 mL liver volume in 60 minutes (at a speed of 1mL/min) with decreasing ablation times expected after parameter optimization. Additionally, we have obtained the following data in a murine subcutaneous HCC model and rodent liver model5: 1) effective tumor volume reduction and significantly lengthened survival time; 2) Histotripsy-produced acellular homogenate completely absorbed in one month; 3) significant histotripsy-stimulated immune response at the local tumor site and distant organs.
Brain tumor treatment
Approximately 256,000 new patients are diagnosed with primary brain tumor annually worldwide, and many more patients are diagnosed with brain metastases. The first-option treatment is craniotomy-based surgical resection, a highly invasive surgery associated with morbidities secondary to surgical trauma as well as retraction-based injury to the surrounding cerebral parenchyma. Radiation therapy is only used as an adjunct treatment, as many brain structures are susceptible to radiation-induced damage. Drug-based therapy has shown limited effect in treating brain tumors due to the impermeability of the blood brain barrier. There is a clear clinical need for a noninvasive, safe, and effective treatment for brain tumors.
Transcranial magnetic resonance guided focused ultrasound (tcMRgFUS) has been investigated for noninvasive ablation to treat neuro-disorders and brain tumors. Guided by MRI, ultrasound is applied from outside the skull and focused to the target brain tissue to produce thermal necrosis, while the surrounding brain and the skull remain intact. tcMRgFUS has been approved by FDA to treat essential tremor by ablating a single focal volume within the central nervous system. However, due to the overheating of the skull, tcMRgFUS cannot treat locations <2 cm from the skull surface, rendering inoperable up to ~90% of the cortex where brain tumors often reside. Moreover, tcMRgFUS cannot treat volumes >1 cm diameter in the brain. These limitations on treatment location and volume are major roadblocks preventing tcMRgFUS from widespread use.
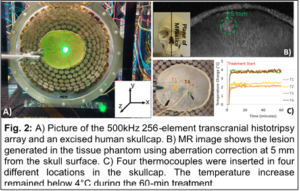
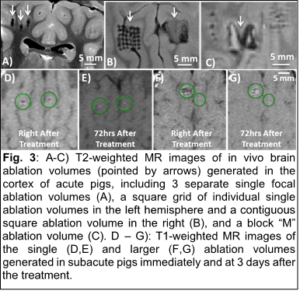
Unlike tcMRgFUS that relies on heating produced by continuous sonication, histotripsy uses microsecond-length ultrasound pulses to generate focal cavitation with millimeter accuracy to liquefy the target tissue into acellular homogenate. With long cooling times between pulses (duty cycle <0.1%), overheating to the skull and surrounding tissue can be avoided, while effectively ablating the target brain tissue. We have constructed a 500kHz and 250kHz 256 element hemispherical array for transducer brain tumor treatment using 3D printing technique. Our preliminary data show the following6-8. 1) Applied through excised human skulls, histotripsy can treat locations from the skull base to 5 mm from the skull surface as well as volume targets (e.g. 3 cm diameter ex vivo bovine brain in 30 minutes), while keeping the temperature increase in the skull under 4°C (Fig. 2). 2) Initial in vivo safety and feasibility was demonstrated in the normal pig brain. Histotripsy was used to create single and contiguous ablation volumes (>1 cm3) in the cortex region. Pathology shows no viable cellular structures within the ablation zone, sharp boundaries (<200 µm), and no damage or hemorrhage beyond the borders (Fig. 3). 3) We have developed specialized MRI sequences and collected preliminary MR images with sufficient image quality to visualize histotripsy-induced cavitation and tissue fractionation in real-time.
In addition to liver and brain tumors, we have previously investigated histotripsy for urology, breast and cardiac applications.
References
- Vlaisavljevich E, Kim Y, Allen S, Owens G, Pelletier S, Cain C, Ives K, Xu Z. Image-guided non-invasive ultrasound liver ablation using histotripsy: feasibility study in an in vivo porcine model. Ultrasound Med Biol. 2013;39(8):1398-409. PMCID: 3709011.
- Vlaisavljevich E, Owens G, Lundt J, Teofilovic D, Ives K, Duryea A, Bertolina J, Welling TH, Xu Z. Non-Invasive Liver Ablation Using Histotripsy: Preclinical Safety Study in an In Vivo Porcine Model. Ultrasound Med Biol. 2017;43(6):1237-51.
- Kim Y, Vlaisavljevich E, Owens GE, Allen SP, Cain CA, Xu Z. In vivo transcostal histotripsy therapy without aberration correction. Phys Med Biol. 2014;59(11):2553-68.
- Smolock AR, Cristescu MM, Vlaisavljevich E, Gendron-Fitzpatrick A, Green C, Cannata J, Ziemlewicz TJ, Lee FT, Jr. Robotically Assisted Sonic Therapy as a Noninvasive Nonthermal Ablation Modality: Proof of Concept in a Porcine Liver Model. Radiology. 2018;287(2):485-93.
- Vlaisavljevich E, Greve J, Cheng X, Ives K, Shi J, Jin L, Arvidson A, Hall T, Welling TH, Owens G, Roberts W, Xu Z. Non-Invasive Ultrasound Liver Ablation Using Histotripsy: Chronic Study in an In Vivo Rodent Model. Ultrasound Med Biol. 2016;42(8):1890-902. PMCID: PMC4912895
- Kim Y, Hall TL, Xu Z, Cain CA. Transcranial Histotripsy Therapy: A Feasibility Study. IEEE Trans Ultrason Ferroelectr Freq Control. 2014;61(4):582-93.
- Sukovich J, Xu Z, Kim Y, Cao H, Nguyen TS, Pandey A, Hall T, Cain C. Targeted Lesion Generation Through the Skull Without Aberration Correction Using Histotripsy. IEEE Trans Ultrason Ferroelectr Freq Control. 2016;63(5):671-82.
- Gerhardson T, Sukovich JR, Pandey AS, Hall TL, Cain CA, Xu Z. Effect of Frequency and Focal Spacing on Transcranial Histotripsy Clot Liquefaction, Using Electronic Focal Steering. Ultrasound Med Biol. 2017;43(10):2302-17. PMCID: 5580808.